Quick answer
The Bristol stool chart is a 1–7 scale for stool form. In general, Types 1–2 lean toward slower transit (constipation pattern), Types 3–4 are often typical, and Types 5–7 lean toward faster transit (diarrhea pattern). The point is not to “hit the perfect number” but to label consistently so you can spot repeat patterns.
How to read the Bristol stool chart (Types 1–7)
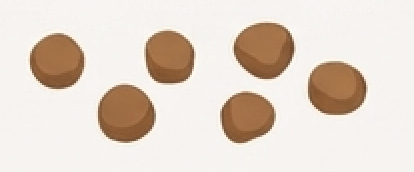
- Types 1–2: often a slow-transit / constipation pattern
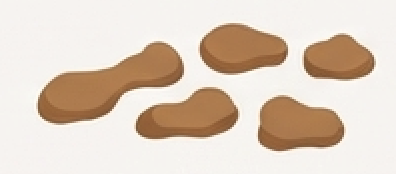
- Types 3–4: often typical stool form
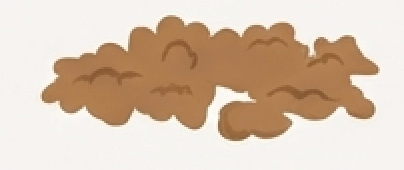
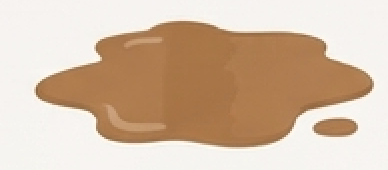
- Types 5–7: often a faster-transit / diarrhea pattern
One practical tip: if you’re stuck between Type 4 and 5, pick the closest and stay consistent for 1–2 weeks. Trend clarity beats perfect labeling.
What can shift your Bristol type (without it meaning “something is wrong”)
Day-to-day variation is common. Usual drivers include:
- routine changes (travel, sleep shifts)
- fiber swings: see Fiber: what it does and how to ramp
- caffeine timing: see Caffeine: what to watch
- dairy/lactose: see Lactose: what to track
- sweeteners/polyols: see Sweeteners and polyols
- new meds/supplements
The goal is not to blame a single food. It’s to notice what repeats.
A practical 7-day baseline + one change
- Track Bristol type + time of day for 7 days without changing habits.
- Add 1–2 tags (don’t overdo it): caffeine timing, fiber, lactose, sweeteners/polyols.
- Pick one lever and test it for 7 days.
- Compare before/after counts rather than single days.
If you want a clean method for testing triggers: How to identify your trigger foods (7-day method).
When to seek care
Stool type alone rarely decides urgency. What matters most is red flags and persistence.
Seek medical care for blood, black/tarry stool, severe pain, fever, faintness, or unexplained weight loss.
Evidence note
The Bristol Stool Form Scale is widely used in clinics and research as a shared language for stool form. It helps describe patterns but does not diagnose conditions on its own.